Irritable bowel syndrome
|
Irritable bowel syndrome (IBS) is a challenging problem for patients and their doctors.
It is a health problem that has no test to prove the diagnosis. This makes many people question the diagnosis despite the fact that it affects the quality of life of so many people. |
Did you know that at least 15% of the world suffers from IBS?
|
Let me try to simplify this complex problem
Facts to focus on
- IBS is a real problem. We do not fully understand it but it is well-recognized as an important health issue.
- Many people suffer from IBS. In fact at least 15% of the population has it. It often first shows up in late teenager years but can appear at any age often triggered by a gastrointestinal infection or a stressful event.
- It does NOT lead to cancer or inflammatory bowel disease. This is a common worry and is absolutely not true.
Typical symptoms of IBS
|
These symptoms can be intermittent or daily.
Often a patient has had these symptoms for many months or even years before seeking help. |
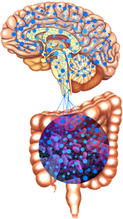
Brain-Gut interaction
|
The brain-gut interaction is the connection between our brain, the enteric nervous system and the intestinal bacteria. We are still in the infancy of understanding this complex interaction.
The enteric nervous system is the "brain" of our digestive system. Just like a brain, it controls how the digestive system moves or contracts and how it feels and senses stimuli. The bacteria in our colon can influence how the enteric nervous system behaves. The field of gut microbiome research is trying to understand the role bacteria play in heath and disease but we still have so much to learn. Our brains receive messages from our digestive system to let us know if things are working properly but it can also change how the digestive system is working. |
What does this all mean?
This means that IBS is a combination of a problem of the brain, the enteric nervous system and the intestinal flora. To attempt to fix it means all 3 parts may need to be addressed.
How can I be sure it is not something else?
You are right that all the typical symptoms can also be seen in other diseases such as IBD, celiac disease and colon cancer.
Most of the time, in fact well over 90% of the time, your doctor can make an accurate diagnosis of IBS just on your story.
There are alarming features that if present may not be suggestive of IBS and may prompt more investigation.
Most of the time, in fact well over 90% of the time, your doctor can make an accurate diagnosis of IBS just on your story.
There are alarming features that if present may not be suggestive of IBS and may prompt more investigation.
Alarming symptoms
- Blood loss - Of course fresh blood from the rectum could be just hemorrhoids but it should be checked.
- Vomiting frequently
- Weight loss - a certain amount of weight loss is normal if someone changes their diet because of IBS but anything beyond 10-15 lbs needs to be checked.
- Severe focal abdominal pain - IBS pain tends to be more generalized.
- Family history of other digestive diseases
- Blood test abnormalities
|
Once I suspect that the patient has IBS, the only tests I perform outside of a physical exam are:
If any of these tests are positive, I would proceed with further tests such as a colonoscopy or x-ray imaging. |
What is the treatment for IBS?
|
Treatment focuses on 3 different levels
1. Education 2. Diet 3. Medication |
Remember that each patient has different symptoms and needs so treatment has to be individualized for each patient
|
Education
|
Educating a you about IBS helps you understand the symptoms you are experiencing and decreases the worry and anxiety associated.
|
Diet
There are a variety of diet modifications that can be helpful. More information can be found in the diet section.
I want to focus on a few pertinent points.
Besides the food that you eat, you also need to pay attention to how you eat.
I want to focus on a few pertinent points.
Besides the food that you eat, you also need to pay attention to how you eat.
- take time to eat more slowly to allow for better digestion
- eat roughly the same amount and at the same time each day so that your digestive system develops a predictable rhythm.
- pay attention to your mood. The IBS symptoms that day may have had more to do with your mood then the foods that you ate
Medication

There are many medications both prescription, over the counter and herbal that have been used in the treatment of IBS.
The problem with figuring out what is effective is that there is a very high placebo response rate for medications used in IBS. A placebo response is when a patient improves with a treatment that has no active medication such as giving a sugar pill. In fact the placebo response rate can be sometimes over 50%! This is why every treatment in IBS must be compared to a placebo to see if the improvement is really as a result of the medication itself.
Lets discuss briefly the different available products.
Over the counter:
Most over the counter medications do not do much. The simethicone products meant to decrease gas and bloating have little value. Bismuth in Pepto Bismol can help to decrease bloating, gas and diarrhea during an attack but should not be used regularly due to risk of side effects.
A new treatment called IBgard has shown to be beneficial for abdominal discomfort, bloating and urgency. IBgard is peppermint oil that has been packaged to reduce the side effects of nausea and reflux.
Antispasmodics:
Both pinaverium (Dicetel) and trimebutine (Modulon) are considered anti-spasm medications that have shown mild benefit in IBS. They are used widely more because they have little side effects than their true benefit. They are usually prescribed as a daily medication taken 2-3 times per day.
Anticholinergic drugs such as dicyclomine (Bentylol) or hycosine butylbromide (Buscopan) are good for on the spot treatment to abort abdominal cramps. Taken regularly can lead to decrease effect of the medication and side effects such as constipation and dry mouth so best to use intermittently. It can take several minutes to see the full effect so best to take it early.
Probiotics:
It would seem logical to try to alter the bacterial flora with a probiotic but at this point in time, there is not enough data to help us know which probiotic to use, how much and how long. Since it is relatively harmless, it is worth trying a probiotic for 1-2 months to se if there is any benefit.
Antidepressants:
Antidepressants play a valuable role in modifying the abnormal response of the enteric nervous system and the brains reaction to these responses. The best studied type of antidepressants in IBS is the tricyclic antidepressants (TCA) although the selective serotonin reuptake inhibitors (SSRI) have also shown to be beneficial.
The TCA are usually prescribed at a low dose that cannot treat depression but that minimizes dramatically the potential side effects. The SSRI are prescribed at the typical dosage as for depression or anxiety.
There are 2 medications for constipation predominant IBS that not only improve constipation but that improve the IBS symptoms of bloating and cramps.
Prucalopride (Resotran) is a 5-HT4 receptor agonist that increases intestinal motility and decreases intestinal hypersensitivity. The usual dose is 2 mg per day although it should be reduced to 1 mg in elderly patients.
Linaclotide (Constella) stimulates secretion of chloride and bicarbonate and water into the intestinal lumen to decrease constipation but also decreases intestinal sensitivity. The usual dose is 290 mg per day.
Both have low side effect profile with the main side effect being diarrhea. Some patients can have quite a dramatic diarrhea at the start so I always recommend starting these medications when you are home.
I will prescribe both for 3 months as the constipation relief may be seen as early as one week but the improvement in cramps and bloating can take up to 3 months.
There is a new treatment for diarrhea predominant IBS called eluxadoline (Viberzi). Eluxadoline acts upon the opioid receptors influencing the enteric nervous system. It will improve diarrhea and decrease intestinal sensitivity.. The usual dose is 100 mg twice daily. The side effect profile is low but there is a risk of pancreatitis in patients who have had their gallbladder removed or who drink more than 3 drinks of alcohol per day. Alosetron (Lotronex) is another drug marketed for diarrhea predominant IBS but it is not available in Canada.
Rifaximin is a non-absorbed antibiotic that has been shown to have benefit in diarrhea predominant IBS. This was originally based on studies that suggested that some patients with IBS have small intestinal bacterial overgrowth (SIBO). The role of SIBO in IBS has been highly questionable and has created a lot of controversy. I am not convinced at this time that SIBO plays a role in IBS. That being said many antibiotics can change the intestinal flora and will lead temporarily to improvement and even sometimes worsening of IBS. Since Rifaximin is not absorbed it would be safer to use in IBS than other antibiotics. How often we can treat with Rifaximin is not yet known.
The problem with figuring out what is effective is that there is a very high placebo response rate for medications used in IBS. A placebo response is when a patient improves with a treatment that has no active medication such as giving a sugar pill. In fact the placebo response rate can be sometimes over 50%! This is why every treatment in IBS must be compared to a placebo to see if the improvement is really as a result of the medication itself.
Lets discuss briefly the different available products.
Over the counter:
Most over the counter medications do not do much. The simethicone products meant to decrease gas and bloating have little value. Bismuth in Pepto Bismol can help to decrease bloating, gas and diarrhea during an attack but should not be used regularly due to risk of side effects.
A new treatment called IBgard has shown to be beneficial for abdominal discomfort, bloating and urgency. IBgard is peppermint oil that has been packaged to reduce the side effects of nausea and reflux.
Antispasmodics:
Both pinaverium (Dicetel) and trimebutine (Modulon) are considered anti-spasm medications that have shown mild benefit in IBS. They are used widely more because they have little side effects than their true benefit. They are usually prescribed as a daily medication taken 2-3 times per day.
Anticholinergic drugs such as dicyclomine (Bentylol) or hycosine butylbromide (Buscopan) are good for on the spot treatment to abort abdominal cramps. Taken regularly can lead to decrease effect of the medication and side effects such as constipation and dry mouth so best to use intermittently. It can take several minutes to see the full effect so best to take it early.
Probiotics:
It would seem logical to try to alter the bacterial flora with a probiotic but at this point in time, there is not enough data to help us know which probiotic to use, how much and how long. Since it is relatively harmless, it is worth trying a probiotic for 1-2 months to se if there is any benefit.
Antidepressants:
Antidepressants play a valuable role in modifying the abnormal response of the enteric nervous system and the brains reaction to these responses. The best studied type of antidepressants in IBS is the tricyclic antidepressants (TCA) although the selective serotonin reuptake inhibitors (SSRI) have also shown to be beneficial.
The TCA are usually prescribed at a low dose that cannot treat depression but that minimizes dramatically the potential side effects. The SSRI are prescribed at the typical dosage as for depression or anxiety.
There are 2 medications for constipation predominant IBS that not only improve constipation but that improve the IBS symptoms of bloating and cramps.
Prucalopride (Resotran) is a 5-HT4 receptor agonist that increases intestinal motility and decreases intestinal hypersensitivity. The usual dose is 2 mg per day although it should be reduced to 1 mg in elderly patients.
Linaclotide (Constella) stimulates secretion of chloride and bicarbonate and water into the intestinal lumen to decrease constipation but also decreases intestinal sensitivity. The usual dose is 290 mg per day.
Both have low side effect profile with the main side effect being diarrhea. Some patients can have quite a dramatic diarrhea at the start so I always recommend starting these medications when you are home.
I will prescribe both for 3 months as the constipation relief may be seen as early as one week but the improvement in cramps and bloating can take up to 3 months.
There is a new treatment for diarrhea predominant IBS called eluxadoline (Viberzi). Eluxadoline acts upon the opioid receptors influencing the enteric nervous system. It will improve diarrhea and decrease intestinal sensitivity.. The usual dose is 100 mg twice daily. The side effect profile is low but there is a risk of pancreatitis in patients who have had their gallbladder removed or who drink more than 3 drinks of alcohol per day. Alosetron (Lotronex) is another drug marketed for diarrhea predominant IBS but it is not available in Canada.
Rifaximin is a non-absorbed antibiotic that has been shown to have benefit in diarrhea predominant IBS. This was originally based on studies that suggested that some patients with IBS have small intestinal bacterial overgrowth (SIBO). The role of SIBO in IBS has been highly questionable and has created a lot of controversy. I am not convinced at this time that SIBO plays a role in IBS. That being said many antibiotics can change the intestinal flora and will lead temporarily to improvement and even sometimes worsening of IBS. Since Rifaximin is not absorbed it would be safer to use in IBS than other antibiotics. How often we can treat with Rifaximin is not yet known.
Alternative treatments
Acupuncture, hypnotherapy, yoga and exercise have all been shown to assist in the management of IBS.
Other treatments such as herbal, Chinese or homeopathic treatments may help some patients but have been poorly studied often without checking for a placebo response.
Other treatments such as herbal, Chinese or homeopathic treatments may help some patients but have been poorly studied often without checking for a placebo response.

I focus most of my effort on educating my patients and arriving at a reasonable expectation.
I will always discuss dietary modification and its role in helping decrease the intestinal sensitivity and the bacterial flora. I usually recommend doing the low FODMAP. I recommend doing it strictly for 1 month and then gradually reintroducing food groups. The benefit of the 1 month trial is firstly to see if diet modification will even work and secondly to allow time for the intestinal sensitivity to be downgraded.
I will discuss the influence of stress on IBS symptoms and often discuss the value of seeing a psychologist for stress management.
I do not suggest the over the counter products often although my experience with IBgard is new.
I do use Buscopan or Bentylol often for patients who suffer from severe cramps intermittently. The usual dose is 10 mg as needed.
I use tricyclic antidepressants frequently. I use most commonly nortryptilline or desipramine at doses of 25-50 mg daily. I give it at night to help in sleep that is often disturbed in patients with IBS. I will use the SSRI antidepressants especially in patients with a strong anxiety component but I will encourage professional psychological help at the same time.
I have used both prucalopride and linaclotide for constipation predominant IBS but typically after a failure of laxatives.
I will always discuss dietary modification and its role in helping decrease the intestinal sensitivity and the bacterial flora. I usually recommend doing the low FODMAP. I recommend doing it strictly for 1 month and then gradually reintroducing food groups. The benefit of the 1 month trial is firstly to see if diet modification will even work and secondly to allow time for the intestinal sensitivity to be downgraded.
I will discuss the influence of stress on IBS symptoms and often discuss the value of seeing a psychologist for stress management.
I do not suggest the over the counter products often although my experience with IBgard is new.
I do use Buscopan or Bentylol often for patients who suffer from severe cramps intermittently. The usual dose is 10 mg as needed.
I use tricyclic antidepressants frequently. I use most commonly nortryptilline or desipramine at doses of 25-50 mg daily. I give it at night to help in sleep that is often disturbed in patients with IBS. I will use the SSRI antidepressants especially in patients with a strong anxiety component but I will encourage professional psychological help at the same time.
I have used both prucalopride and linaclotide for constipation predominant IBS but typically after a failure of laxatives.
|
www.ourdigestivehealth.com
www.GadFriedman.com |